Click on the links below to find out more about
Direct Anterior/Bikini Total Hip Replacement Surgery
Click on the links below to find out more about
Direct Anterior/Bikini Total Hip Replacement Surgery
OVERVIEW
Having your hip replaced comes with both positives and negatives. However, when the alternative is living a lower quality of life due to pain, stiffness, and reduced motion, opting for surgery is often the best choice for many patients. The anterior approach for hip replacement involves making a small incision and inserting the new hip joint READ MORE .
It’s a minimally invasive technique that circumvents the need to cut through muscle and tendons, drastically improving overall healing time. Dr David Slattery, a renowned hip specialist, is skilled in the precision work involved with anterior hip replacements. The anterior incision for hip replacements is around 8cm and is located in front of the hip. This technique avoids cutting muscle, and it takes a skilled hand to complete the surgery. This approach also allows for X-rays during the procedure to guide accurate implant positioning and reduce complications.
Posterior hip replacements are more common. Despite an extended recovery time due to surgically cutting the muscles and tendons to insert the replacement hip, this surgery is not as technically demanding as anterior hip replacement surgery.
The anterior incision for hip replacement is much smaller than for posterior surgery. By making an 8cm incision (anterior) rather than 15-20cm (posterior), the post-surgery wound is smaller. It’s also located on the front of your hip, rather than on the buttocks, which may make a difference to your comfort during the recovery phase.
Another of the advantages of anterior hip replacement is the avoidance of cutting through muscle and tendons. Skilled surgeons are able to insert your new hip without causing traumatic damage to the surrounding tissue and muscles. There is an extended recovery period associated with the posterior approach, compared with the anterior approach, because of this additional damage. Furthermore, the muscles can become weaker resulting in reduced hip stability. However, as the anterior approach hip replacement surgery avoids this problem, recovery can begin much faster.
The anterior approach to the hip joint was first described in 1881 for draining infected hips, and was first used for joint replacement in France approximately 40yrs ago. It involves going between the muscles, rather than cutting them. It is a technically difficult approach that was largely refined by Joel Matta in the USA and Frederic Laude in Paris with the introduction of specialised instrumentation and techniques to make it easier to place large total hip implants through a small incision (8-10cm) at the front of the hip.
Potential advantages of anterior total hip replacement:
Potential disadvantages:
The Posterior Approach was developed later and this largelysolved the problems of tendon and bone healing of the Hardinge and Lateral Approaches. It involves an incision 15-20cm long which is curved over the buttock. It involves splitting the Gluteus Maximus muscle and cutting the small muscles which attach to the back of the hip joint. This is an excellent approach which can easily be extended and is the approach of choice for complex total hip replacement and revision procedures. Potential problems associated with this approach include:
Dr David Slattery is skilled and has extensive experience in both anterior and posterior surgeries, with around most of hip replacements performed through the anterior method.
When it comes to choosing the method, each patient case is reviewed on individual merits. Attention is paid to your overall health and any other specific health concerns are also considered during the decision-making process. If you have a preference, please discuss this during your consultation with Dr Slattery. It may, however, be the case that this preferred method is incompatible with other health issues. Dr Slattery will fully discuss these with you, if appropriate.
If you would like to be assessed by renowned hip specialist Dr David Slattery for a total hip replacement and are interested in the advantages of anterior hip replacement, please complete our online booking form. Alternatively, you can call one of Dr Slattery’s consulting locations to make an appointment and ask any questions that you may have READ LESS .
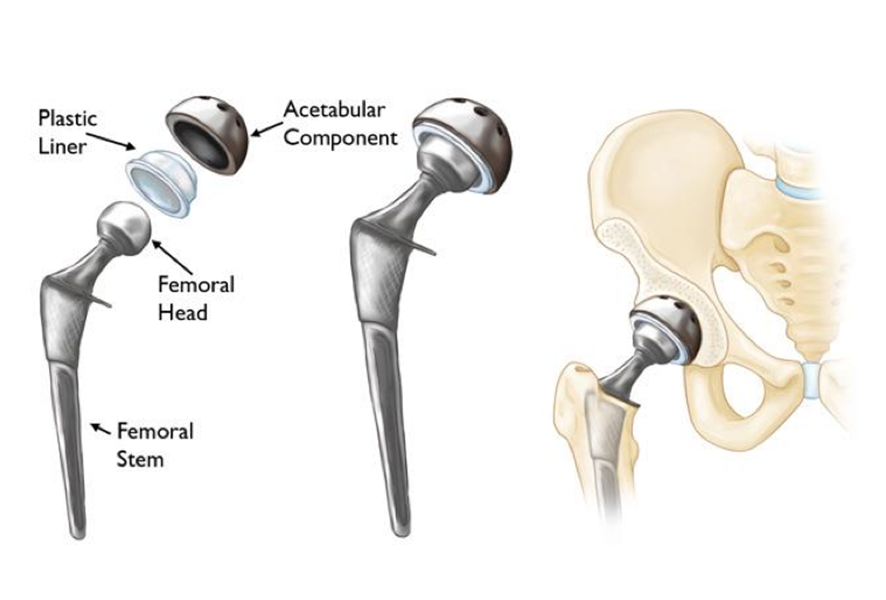
There are normally four components to a total hip replacement:
A standard hip replacement in Australia refers to a hip replacement performed using an incision over the side of the hip with access to the hip joint from the back (posterior). It involves splitting various muscles to gain access to the hip joint. It offers excellent exposure of the hip, and is routinely done across Australia. Variations of this “standard” approach practiced by Australian surgeons are the Direct Superior Approach (DSA), and SuperPATH® hip replacement techniques, which still cut varying amounts of muscle tissue.
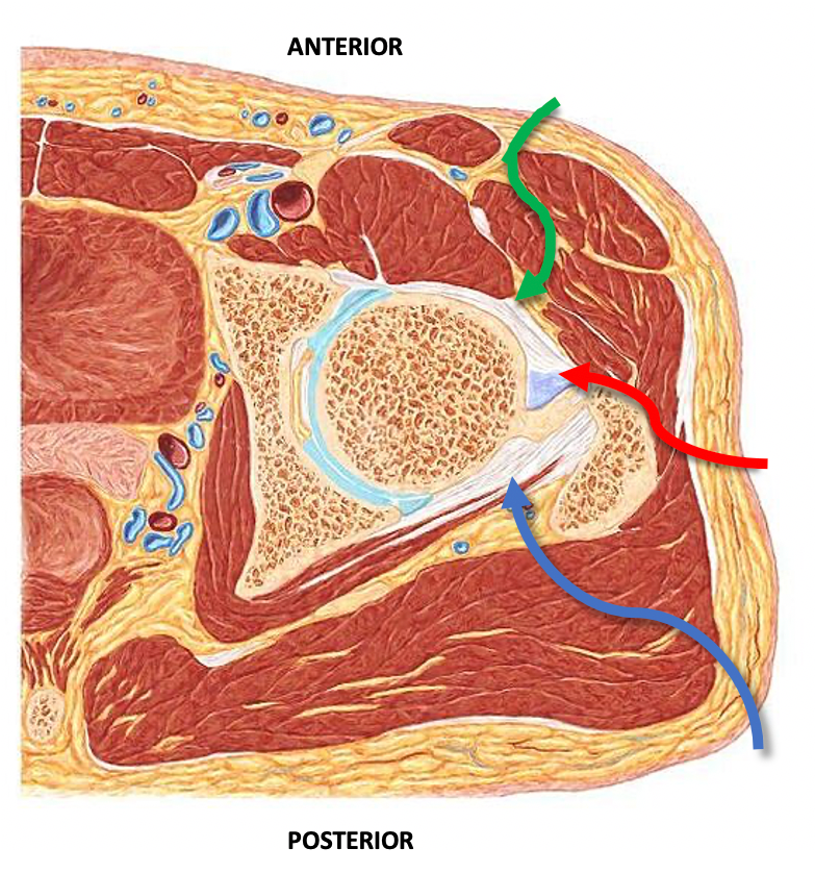
An anterior hip replacement is a hip replacement from the front of the hip, which involves an incision in the groin as opposed to the side. This approach for hip replacement was originally described in Europe, and has gained popularity in the United States. More recently it has gained popularity in Australia.
Dr Slattery uses either a cosmetic, or bikini, incision in the groin crease or an oblique incision which results in a small scar in the groin approximately 8-10cm long in most cases. The operation goes between muscles rather than cutting through them, which reduces the amount of trauma to the soft tissues and preserves the normal anatomy. The goals of anterior hip replacement are:
FAQs for hip replacement surgery
Should I have a hip replacement?
There are many things to consider when making a decision to undergo hip replacement surgery. It could ultimately give you relief from chronic pain and suffering, but there could also be an alternative. It is always best to be armed with plenty of questions ahead of your initial consultation with your hip replacement specialist.
What is the recovery time on an anterior hip replacement surgery?
Most patients are sitting out of bed or standing on the first day after surgery. Some patients are able to walk and can be safely discharged home in 36-72hrs. Usually patients will resume most normal activities within 3 – 6 weeks of their total hip replacement surgery. Once activity is possible with minimal pain, physical therapy and light exercise will be important to incorporate as a way to help recovery.
What are the complications with anterior hip replacement surgery?
This type of surgery is considered safe and is highly effective for patients who require it. With any surgery there can be complications and for hip surgery you may encounter the following:
Many steps are taken at each step of your operation to prevent complications occurring, and overall hip replacement is very safe and effective.
What can I expect after hip replacement surgery?
You will spend 2-3 days in hospital afterwards and be advised on how best to take care during the recovery period. Within the first few days you will be encouraged to walk with assistance from physiotherapy and nursing supports. Most patients do not need to go to inpatient rehabilitation post op unless they have significant medical co-morbidities or no supports at home.
Following surgery you will be required to avoid driving for approximately 2 weeks, possibly longer, depending on how quickly you regain confidence and coordination.
Ongoing pain from a hip replacement can be expected in the first few weeks. This should subside as your recovery time and postoperative physical therapy is undertaken.
What activities should I avoid after hip replacement surgery?
Patients should avoid driving for 2 weeks after hip replacement surgery (at a minimum). There are no other restrictions upon your activities after an anterior hip replacement.
Is hip replacement surgery safe?
Hip replacement surgery has a long proven safety record over many decades. With constant refinement techniques have become better to prevent short and long term problems. Advances in technique and materials have ensured that surgeries performed today are safer and deliver longer-lasting benefits to a greater number of patients than ever before. Dr Slattery prioritises the safety of his patients at every step of their journey to health, ensuring that the risk of complications such as blood clots and nerve damage are minimised.
How long will my new joint last after hip replacement surgery?
New, stronger artificial joints and improvements in implant delivery and placement mean that more than 85% of all hip joint implants will last 20 years without revision.


Dr Slattery is a hip replacement specialist located in Melbourne and has learnt the intricacies of Direct Anterior Total Hip Replacement surgery in both Switzerland and Australia from world leaders in this technique. Additionally, he provides hip replacement keyhole surgery (arthroscopy) where suitable for patients. He now has a number of total hip replacement consulting rooms across Melbourne.
Patient selection is extremely important in ensuring that you get the best outcome from your hip replacement surgery. Dr Slattery will assess you individually and discuss the best option for you during your consultation.
To book a consultation with Dr Slattery, a hip replacement specialist in Melbourne, please contact one of his rooms listed here, or by using our online contact form.